Research labs by now have established that the virus that causes coronavirus disease 2019 (COVID-19) is stable for several hours to days in aerosols and on surfaces.
Scientists found that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was detectable in aerosols for up to three hours; up to four hours on copper; up to 24 hours on cardboard; and up to two to three days on plastic and stainless steel. This study by the National Institutes of Health, CDC, UCLA and Princeton University scientists was published in The New England Journal of Medicine.
The study also shows that in contrast to SARS-CoV-1, which caused Severe acute respiratory syndrome (SARS), most secondary cases of virus transmission of SARS-CoV-2 (which causes COVID-19 disease) appear to be occurring in community settings rather than healthcare settings.
The good news
Even as we digest this uncomfortable news, and take preventive action as directed by the Centers for Disease Control and Prevention (CDC) and by other methods, there’s some positive news–our immune system can fight back.
Melbourne researchers have mapped immune responses from one of Australia’s first novel COVID-19 patients, showing the body’s ability to fight the virus and recover from the infection. Their report has been published in Nature Medicine.

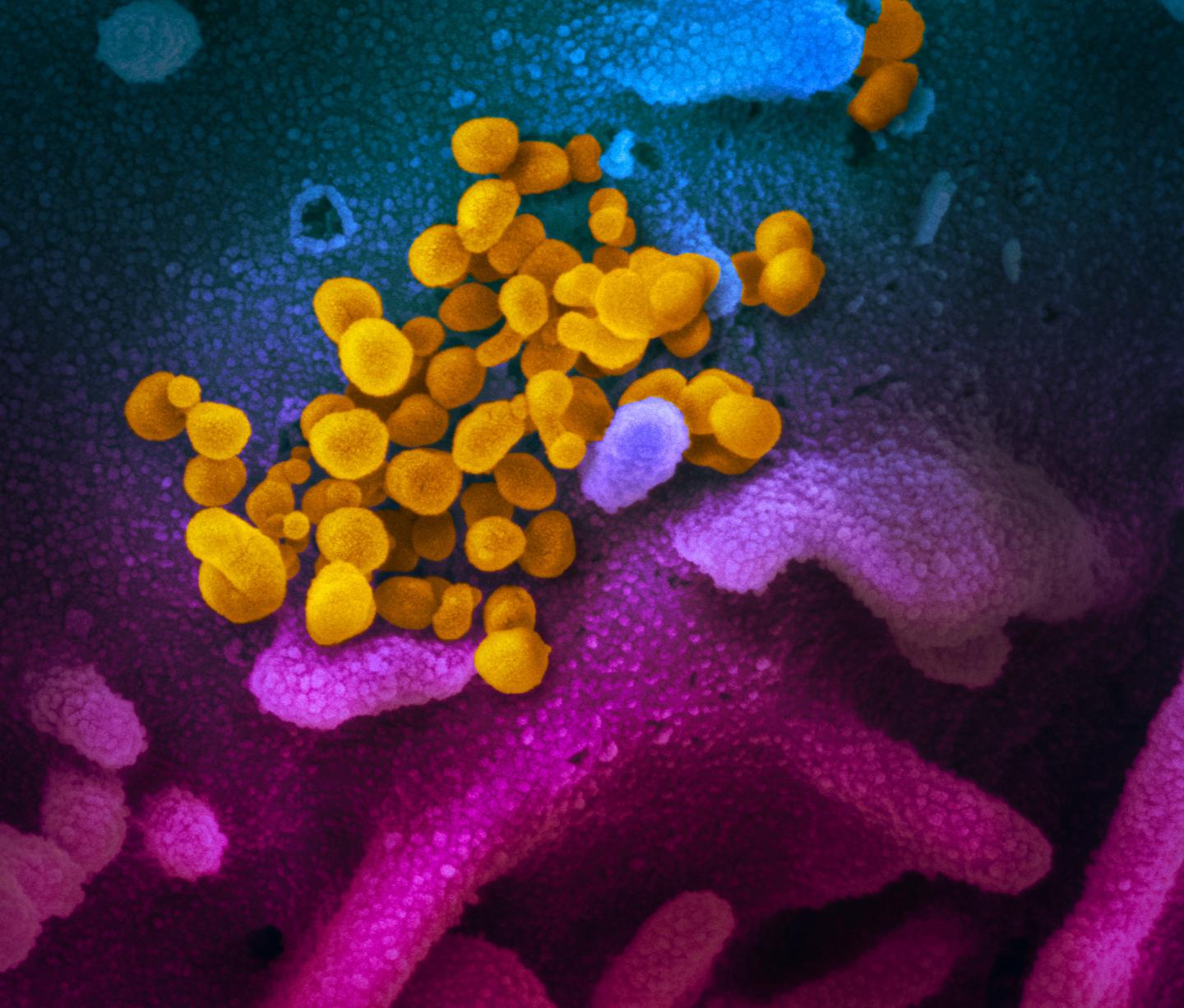
CREDIT: NIAID RML
Researchers at the Peter Doherty Institute for Infection and Immunity (Doherty Institute)–a joint venture between the University of Melbourne and the Royal Melbourne hospital–were able to test blood samples at four different time points in an otherwise healthy woman in her 40s, who presented with COVID-19 and had mild-to-moderate symptoms requiring hospital admission.
“Three days after the patient was admitted, we saw large populations of several immune cells, which are often a tell-tale sign of recovery during seasonal influenza infection, so we predicted that the patient would recover in three days, which is what happened,” said one of the authors on the paper, research fellow Dr Oanh Nguyen.
The research team was able to do this research so rapidly thanks to SETREP-ID (Sentinel Travellers and Research Preparedness for Emerging Infectious Disease), led by Royal Melbourne Hospital Infectious Diseases Physician Dr Irani Thevarajan at the Doherty Institute.
SETREP-ID is a platform that enables a broad range of biological sampling to take place in returned travelers in the event of a new and unexpected infectious disease outbreak, which is exactly how COVID-19 started in Australia.
Dr Thevarajan said current estimates show more than 80 per cent of COVID-19 cases are mild-to-moderate, and understanding the immune response in these mild cases is very important research.
“We hope to now expand our work nationally and internationally to understand why some people die from COVID-19, and build further knowledge to assist in the rapid response of COVID-19 and future emerging viruses,” she said.
According to University of Melbourne Professor Katherine Kedzierska–a laboratory head at the Doherty Institute and a world-leading influenza immunology researcher–the team was able to dissect the immune response leading to successful recovery from COVID-19, which might be the secret to finding an effective vaccine.
“We showed that even though COVID-19 is caused by a new virus, in an otherwise healthy person…People can use our methods to understand the immune responses in larger COVID-19 cohorts, and also understand what’s lacking in those who have fatal outcomes,” Professor Kedzierska said.